Automate Medicaid processing and financial reviews to make smarter Medicaid determinations
Complete five-year lookbacks for medicaid processing with ease and efficiency
Elder law attorneys and Medicaid processors use Ocrolus technology to automate bank statement analysis for Medicaid eligibility.
Ocrolus empowers you to extract key data from five years of Medicaid documents quickly and accurately. Ocrolus automation enables you to improve program integrity and get benefits to those who need them fast.
Modernize Medicaid application processing with automation and superior analytics
Seamlessly capture data from Medicaid-required documents like bank statements, brokerage statements, and tax documents
Identify high value transactions, transfers, and income sources
Make faster and more informed decisions for Medicaid eligibility
Optimize labor resources to scale with Medicaid application demand
Eliminate manual data entry
Say goodbye to document-review backlogs
Process more Medicaid applications without additional labor
Efficiently determine Medicaid eligibility, fight fraud, and improve program integrity
Boost compliance with standardized financial eligibility reviews
Avoid approving ineligible or fraudulent Medicaid applicants
Ensure applicants move quickly through the Medicaid process
Ready to go?
Discover how to automate and simplify your Medicaid application processing with Ocrolus.

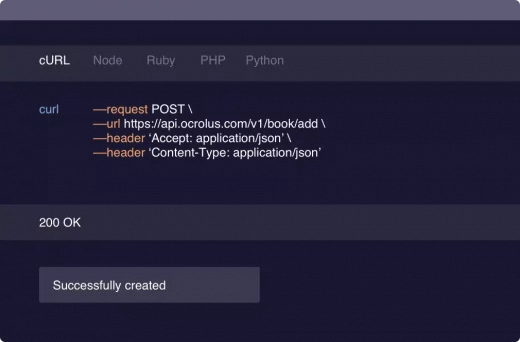
Explore our API
Review our API documentation including guides, references, and tutorials, and see what it’s like to work with Ocrolus.
Frequently Asked Questions
Elder law attorneys and Medicaid processors generally use Ocrolus to automate their medicaid application processing and financial reviews.
Ocrolus improves the speed, efficiency, and accuracy of Medicaid processing. Ocrolus extracts key data from up to five years of Medicaid documents, then reviews and verifies the data, and detects potential application fraud, enabling Medicaid processors to efficiently determine Medicaid eligibility.




